Important: Demonstration Site
This PEUGIC project portal is a mock-up for demonstration purposes. It only contains made-up patient data; you MUST NOT enter real data here.
Duty of candour guidance
Jump to:
- Introduction
- PEUGIC categorisation and “avoidability”
- PEUGIC definition
- Duty of candour - key principles
- Discharging duty of candour
- Case examples
Introduction
The duty of candour is a statutory (legal) duty to be open and honest with patients (or ‘service users’), or their families, when something goes wrong that appears to have caused or could lead to significant harm in the future. It applies to all health and social care organisations registered with the regulator, the Care Quality Commission (CQC) in England.
Discharging duty of candour should be considered if the PEUGIC was probably or definitely avoidable, and if the patient has been harmed by the delay in diagnosis of cancer, or failure to prevent cancer. It is not always possible to be categoric about whether an event is avoidable or whether major harm has occurred. Clinical teams are strongly advised to follow local policies and discuss cases they think might require discharge of duty of candour with the relevant team in their organisation.
This document outlines the key principles, recommends an approach and provides case examples. For further information, please consult the duty of candour guidance published by the CQC.
PEUGIC categorisation and “avoidability”
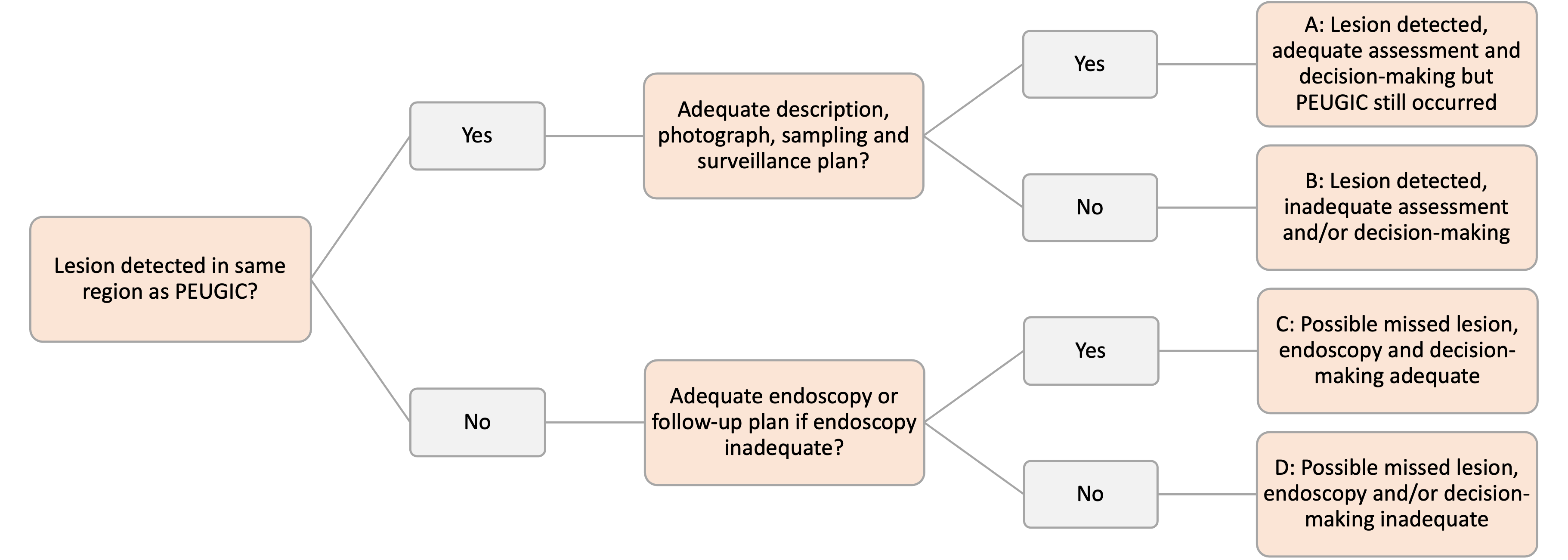
This framework pre-supposes that it was possible for the index endoscopy to have diagnosed or prevented the PEUGIC.
It does not account for all possibilities beyond the control of the endoscopist (such as booking failures) or beyond the control of the service (such as patient choice not to have a repeat procedure or patient unfit for further procedures).
Very small PEUGICs may not have been present or visible at the index endoscopy. Where there is evidence of a cancer associated (e.g. gastric ulcer), pre-malignant (e.g. Barrett’s) or focal potentially malignant lesion at the index endoscopy that was not managed appropriately, this would be deemed avoidable and duty of candour may apply depending on whether there was harm to the patient.
Where there is no cancer associated, pre-malignant or focal lesion described, it will be difficult to be certain whether a lesion was present at the initial endoscopy. In a few cases, endoscopic image review may reveal a lesion that was missed by the endoscopist. For very small cancers, after a long interval the chance of a lesion on the prior test is less likely. Conversely, a large malignancy after a short interval will almost certainly have been there and missed at the initial test. There will be a lot of uncertainty between these extreme examples, and until more is known about the natural history of these cancers we cannot be prescriptive in advice about discharging duty of candour. We recommend discussions about avoidability should be conducted within a “blinded” group of endoscopists, with involvement of risk management teams if deemed appropriate.
PEUGIC definition
The WEO (World Endoscopy Organization) defines an interval cancer as one that has been diagnosed before the next recommended interval (surveillance) endoscopy. Cancers that are diagnosed >3 months and <3 years after an endoscopy that does not show cancer are termed post-endoscopy upper GI cancers (PEUGICs). All interval cancers are PEUGICs but not all PEUGICs are interval cancers and there are three types of non-interval PEUGICs (see table below).
Surveillance is offered to high-risk groups to:
- detect early-stage cancer
- prevent cancer
If cancer appears before, at, or after a planned surveillance interval, it will usually fall within the three-year interval of the project. The local root cause analysis (RCA) pilot performed by Kamran et al found that 40% of PEUGICs were in high-risk groups undergoing surveillance.
We advise audit teams to assume surveillance can prevent cancer in most instances and review each case for the quality of the index endoscopy, and all other facets of management.
The RCA pilot identified shortcomings in quality of procedure, decision making, and booking.
The following table presents possible ‘verdicts’ for hypothetical examples of PEUGICs in surveillance programmes:
| PEUGIC definition | Interval type | Non-interval type A | Non-interval type B | Non-interval type C |
|---|---|---|---|---|
| Recommendation | Detected before recommended interval | Detected at recommended interval | Detected after recommended interval | No interval recommended |
| Index endoscopy findings | Barret’s oesophagus maximum length 2cm, no dysplasia on histology | Barrett’s oesophagus maximum length 5cm, no dysplasia on histology | Gastric atrophy and non-visible low grade dysplasia in stomach | Normal endoscopy |
| Recommendation | Surveillance in 3 years | Surveillance in 3 years | Surveillance in 1 year | No surveillance |
| Outcome | 30 months later develops dysphagia; diagnosis oesophageal cancer | Oesophageal cancer found at surveillance endoscopy | Patient misses appointment, returns 2 years later with gastric cancer | Attends 28 months later with weight loss, repeat endoscopy reveals gastric cancer |
| Possible verdict | The recommended interval may be too long or missed lesion | The recommended interval may be too long or missed lesion | Patient failed to adhere to recommended interval or missed lesion | Fast growing cancer or missed lesion |
Duty of candour - key principles
A service should consider ‘discharging’ its duty of candour if:
- The PEUGIC was probably or definitely avoidable
- The patient was moderately or severely harmed by the delay
While in some cases it will be obvious that the PEUGIC was avoidable and that the patient was significantly harmed, it is recognised that in many instances it will not be obvious. When it is not obvious it is recommended that the case is discussed anonymously with a group of experienced endoscopists to gather a collective view.
Services are strongly advised to record the PEUGIC on Datix or equivalent safety reporting systems, and involve their trust safety and legal team if they believe duty of candour should be discharged, or if they are uncertain whether it should.
Discharging duty of candour
Judgments on “avoidability” and the degree of harm (important for duty of candour) are not black and white. It is recommended that the following approach, adapted from guidance by the Royal College of Radiologists for ‘discrepancies’ is followed:
The case is presented anonymously to a group of colleagues (at least three practising endoscopists) with relevant images.
The group is asked two questions:
- Was this PEUGIC avoidable?
- If so, has the patient been moderately or severely harmed?
If there is no agreement on the second question, or any concerns are raised, it is advised that the hospital team responsible for discharges of duty of candour is involved in the judgment.
PEUGICs can be considered unavoidable if:
- The recommended pathway was not followed because the patient declined investigations or was deemed by the responsible clinician to be too frail to proceed with further investigation.
- The patient had a dysplastic lesion detected on index endoscopy and subsequently underwent endoscopic resection with evidence of cancer on histology over three months later, provided the delay was related to patient not clinical or administrative factors.
- The patient was recognised to have a neoplastic lesion but repeated attempts with adequate biopsy sampling, without inappropriate clinical or administrative delay, failed to provide definitive histological evidence of cancer (e.g. patients with gastric linitus plastica).
- They are small PEUGICs and they are growing by < 5 mm/year, as they will have been unlikely to be detectable during the index endoscopy.
All other PEUGICs are considered potentially avoidable.
To assess harm the following criteria should be used:
- Has the delay caused a change of stage of the disease? (CT/imaging report to confirm this)
- Has the modality of treatment changed i.e. from curative endoscopic therapy, surgery or chemoradiotherapy to palliative radiotherapy or chemotherapy or best supportive care
- Has the intent of the treatment changed i.e. from curative to palliative?
- Has the delay resulted in a change in performance status that now precludes treatment options that would have been possible at time of referral (if comorbidities from the beginning precluded curative treatment then this does not count as harm)
Levels of harm:
- None or minor harm: Minor prolongation of symptoms
- Moderate harm: Moderate increase in symptoms, increase in medication or treatment
- Major harm: Major progression of cancer, contributes to death from condition
- Premature death as a result of the PEUGIC: Directly causes death
Case examples
Please note these examples are intended to be a guide and are neither definitive nor exhaustive. These are based on real cases, but details have been modified so that individuals cannot be recognised.
Case 1
Case details
- 60 year old M
- Endoscopy revealed antral gastric ulcer
- PPI course and repeat endoscopy showed healed ulcer
- All histology benign with no dysplasia
- Repeat endoscopy 18 months later requested for IDA
- 2cm ulcerated cancer different area of antrum
- Underwent distal gastrectomy with no nodal metastases
Root cause analysis
- PEUGIC categorisation: C - possible missed lesion, endoscopy and decision making adequate
- Non-interval type C: no surveillance
Duty of candour issues
- Practice: Possible missed lesion. Endoscopist possibly distracted by ulcer
- Avoidable: Unlikely
- Harm: Possibly. Depends on whether there was precursor lesion. Cancer might have been prevented. If lesion/cancer had been recognised then potentially could have had endoscopic resection rather than surgery and prevention of cancer developing.
- Patient outcome different potentially if diagnosed at PEUGIC endoscopy: Yes (endoscopic resection)
- Discharge of DoC: Not recommended
Case 2
Case details
- 64 year old M
- Symptomatic endoscopy for dysphagia
- Incomplete test (upper oesophagus only) due to very poor tolerance; patient withdrew consent
- Barium swallow requested
- Patient DNA barium
- Patient DNA further clinic appointment - GOJ cancer found on CT for worsening symptoms and weight loss 9 months later
- Patient had surgery but node positive requiring adjuvant chemotherapy (long term outcome unknown)
Root cause analysis
- PEUGIC categorisation: C - possible missed lesion, endoscopy and decision making adequate. Deviated from management pathway but appropriate
- Non-interval type C: no surveillance
- Patient DNA further tests and appointments
Duty of candour issues
- Practice: Appropriate clinical management and repeat test requested. Good documentation and correspondence to GP
- Avoidable: Unlikely
- Harm: Yes likely
- Patient outcome different potentially if diagnosed at PEUGIC endoscopy: Yes (no need adjuvant chemo)
- Discharge of DoC: Not recommended
Case 3
Case details
- 70 year old M
- Surveillance endoscopy for C3M3 Barrett’s oesophagus with no lesion. Seattle protocol biopsies revealed indefinite for dysplasia
- 3 year surveillance interval advised
- Cancer found at next surveillance endoscopy
- Undergoes oesophagectomy of T3 poorly differentiated cancer with nodal metastases
Root cause analysis
- PEUGIC categorisation: B - lesion detected, inadequate assessment or decision making
- Non-interval type A
Duty of candour issues
- Practice: Surveillance guidelines not followed/histology report not assessed
- Avoidable: Possible
- Harm: Yes (cancer might have been prevented with adherence to surveillance intervals)
- Patient outcome different potentially if diagnosed at PEUGIC endoscopy: Yes (endoscopic resection not surgery)
- Discharge of DoC: Recommended
Case 4
Case details
- 60 year old F
- Surveillance endoscopy for extensive gastric atrophy and intestinal metaplasia
- No visible lesion or dysplasia on biopsy
- 3 year interval recommended
- 3 years later 18mm stage 1 cancer found
- Resected endoscopically
Root cause analysis
- PEUGIC categorisation: A - lesion detected, adequate assessment and decision making
- Non-interval type A
Duty of candour issues
- Practice: likely missed benign lesion, but small cancer after three years so lesion likely to have been tiny at original endoscopy.
- Avoidable: Possible
- Harm: May have had an avoidable diagnosis of cancer, but prognosis excellent so no lasting harm
- Patient outcome different potentially if diagnosed at PEUGIC endoscopy: No
- Discharge of DoC: Not recommended
Case 5
Case details
- 71 year old F
- Surveillance endoscopy for C5M6 Barrett’s with no lesion or dysplasia on biopsy
- 3 year interval recommended
- 3 years later 2cm cancer found
- Required oesophagectomy - T2 no nodal metastases
Root cause analysis
- PEUGIC categorisation: A - lesion detected, adequate assessment and decision making
- Non-interval type A
Duty of candour issues
- Practice: Possible missed lesion
- Avoidable: Possible
- Harm: Yes as cancer might have been prevented and surgery might have been avoided, but no studies that have shown it is possible to prevent cancer in all patients with Barrett’s. They may have fast growing cancers arising from very small lesions
- Patient outcome different potentially if diagnosed at PEUGIC endoscopy: Yes (endoscopic resection not surgery)
- Discharge of DoC: Not recommended
Case 6
Case details
- 40 year old F with ALD - endoscopy for varices screening
- Poorly tolerated with no obvious varices on limited examination
- No record of decision about repeat or surveillance
- 30 months later presented with dysphagia and T3 oesophageal squamous cell carcinoma but not fit for curative therapy due ALD
Root cause analysis
- PEUGIC categorisation: D - possible missed lesion, endoscopy or decision making inadequate
- Non-interval type C: no interval recommended
Duty of candour issues
- Practice: High risk for SCC due to alcohol. No immediate repeat endoscopy (or further screening) organised
- Avoidable: Possible
- Harm: Yes but could cancer have been resected endoscopically even if seen at initial endoscopy?
- Patient outcome different potentially if diagnosed at PEUGIC endoscopy: Yes (endoscopic resection not palliation?)
- Discharge of DoC: Uncertain for local discussion and recommendation
Case 7
Case details
- 83 year old F (diabetic) 2WW endoscopy for epigastric pain and weight loss
- Limited views in stomach due solid food
- No record of decision about repeat endoscopy
- 18 months later re-presented with pain and more weight loss - on endoscopy advanced cancer in gastric body
- CT liver metastases - treated palliatively
Root cause analysis
- PEUGIC categorisation: D - possible missed lesion, endoscopy or decision making inadequate
- Non-interval type C: no interval recommended
Duty of candour issues
- Practice: No documentation of decision not to repeat endoscopy (food residue blamed on diabetes?)
- Avoidable: Possible
- Harm: Likely given interval and advanced stage but difficult to be absolutely certain
- Patient outcome different potentially if diagnosed at PEUGIC endoscopy: Yes (curative surgery not palliation?)
- Discharge of DoC: Uncertain for local discussion and recommendation
Case 8
Case details
- 65 year old M 2WW endoscopy for dyspepsia
- 2cm gastric polyp/nodule body - two biopsies (worried about clopidogrel?) - LGD with possible HGD
- No record of action on histology
- Re-presented 2 years later via 2WW with gastric cancer
- Underwent total gastrectomy - T3N1, receiving adjuvant chemotherapy (outcome not yet known)
Root cause analysis
- PEUGIC categorisation: B - lesion detected, inadequate assessment or decision making
- Non-interval type C: no interval recommended
Duty of candour issues
- Practice: Positive decision not to repeat not made/documented
- Avoidable: Possible
- Harm: Cancer likely diagnosed earlier if endoscopy had been repeated and potentially suitable endoscopic resection (not surgery)
- Patient outcome different potentially if diagnosed at PEUGIC endoscopy: Yes (endoscopic resection not surgery)
- Discharge of DoC: Recommended